What is pain?
Pain is a complex experience and can be extremely overwhelming to navigate both as a clinician and patient. There is so much information out there but it can be hard to know where to start and who to go to when we need help looking for answers and treatment. This blog will take a quick dive into the history and come back to explain the biopsychosocial framework in which we understand pain today. Part 2 (still to come) will then help navigate the difference between acute and chronic pain and then follow on in part 3 with some practical advice, treatment and equip the reader with knowledge to know when and where to seek help!
Definition:
The latest definition of pain according to the International Association for the Study of Pain (IASP) is: “An unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage.” This definition highlights how pain is a personal experience that is influenced to varying degrees by biological, psychological and social factors. Pain is always both an emotional and sensory experience. Key things to take away from this definition include the following:
- Pain is a personal experience
- Pain is influenced by biological, social and psychological factors
History: The Biomedical Model
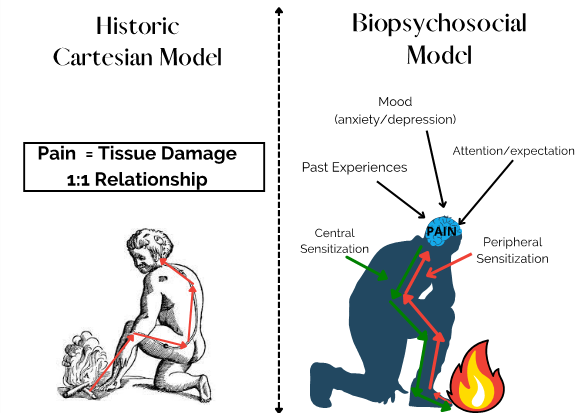
Figure 1: Models of Pain (adapted from thestrengthathlete.com)
-
Nugget 1: Pain does not give us an accurate measurement of tissue damage
Historically, the biomedical approach to pain demonstrated a linear relationship between tissue damage and the pain we experience. This model (proposed by Descartes) is known as the Cartesian model of pain. He taught that the pain we experience is directly proportional to what is happening in our tissues. He proposed that damage to a body part would stimulate neural “pain pathways” sending signals to the brain which would result in pain (in a 1:1 relationship). This understanding of pain attributes all pain experiences to have a physiological cause.
The cartesian model of understanding pain gave rise to the biomedical model which focuses treatments directly on a “cause of pain” which must be found in our tissues. These treatments are often based on biomedical interventions such as medications and surgery. Although this model plays an important role in medicine it cannot explain what is wrong when these medical treatments fail! Sadly this thinking has led many patients, past and present, to be told that their pain is “all in their head”. There are thus huge limitations to this model. Most importantly (as we will explore in later blogs) this model cannot explain why people experience pain beyond the point of normal tissue healing time!
-
Nugget 2: Pain is a Biopsychosocial Phenomenon

Figure 2: Biopsychosocial model of pain (Adams & Turk, 2018)
Thankfully we now can understand pain through the biopsychosocial model (see figure 1). This model has moved away from a more traditional western perspective which is based mainly on biomedical causes which assume this “direct and linear” relationship between sensation, pathology and the pain a person experiences. The biomedical model is majorly flawed as it does not take into account the psychological and social contributions to pain.
Pain is a very dynamic and person-specific process and is influenced by more factors than just what is going on in our tissues. Some of these factors include emotions, sensations, and how we think (cognitions) (Adams & Turk, 2018). Understanding that pain is biopsychosocial gives us lots of treatment options as it highlights that there are many areas (bio, psycho & social) that can be targeted when treating pain.
-
Nugget 3: Pain is a protective response to threat!
We can see how our understanding of pain has come a long way since Cartesian and biomedical models and now we understand that pain is both emotional and sensory and that it is a response to perceived threat in the body. Instead of understanding pain as having a direct 1:1 relationship with tissue damage we understand that pain is modulated by many factors from across the biological, psychological and social domains (G. L. Moseley, 2013). This all might be a bit confusing so let’s look at a practical example.
Think about kicking your toe on a day that is particularly stressful, or when you have a fight with a loved one? Does your pain feel better or worse than on a day where you’re on holiday and having a great time with friends? I’m sure most of us can agree that the pain is worse in the first scenario.
This gives us a clue that pain is not just about tissue damage but that context matters… and if context matters then how we think, feel and behave can affect the amount of pain we feel!
Context can be both evaluative and social. This means it includes both the social situation we are in (are we in a group of friends, a safe environment etc.) and how we perceive the painful experience (our previous pain experiences – maybe last time you kicked your toe you actually broke it?, or you were having a really stressful week?). These things all influences how much pain we experience (L. Moseley, 2003).
Contrary to what Descartes taught (and is still taught today in many places) we do not have “pain pathways” and “pain receptors” in our bodies. Our tissues have special receptors (called nociceptors) which respond to touch, heat, cold and to movement. When these receptors are activated in response to a threat (for example when you kick your toe) messages are sent to the spinal cord and then to the brain where the message is interpreted by the brain.
-
Nugget 4: The brain makes the final decision

Figure 3: The Brain as a volume dial
The brain produces pain once it has interpreted all the contextual factors. The brain is always working subconsciously to interpret the input from the environment (external) and the body (internal). Pain is then created as an output once it has weighed up the information and decided how threatening the experience is.
Think about the toe example once again: Your brain processes the environmental context, past experiences, emotions at the time, understanding of pain and once it has taken all this information into account it produces pain. In the scenario where you are upset/anxious/scared etc. the brain produces more pain as the threat is higher and ultimately more pain is created. Vice versa this explains why we may experience less pain on a day where things are going well and we are with a group of friends!
Picture a volume dial on a TV. The brain functions a little like this. If there is more “threat” perceived by the brain it turns the pain volume up! If there is less “threat” then the volume is turned down and less pain is experienced.
So how do we influence this volume dial? Pain is adaptive and protective but it can also become maladaptive and cause more harm than good. This is what happens when we experience chronic pain. To really understand chronic pain we need to dive into the differences between chronic and acute pain and then we can look at what can be done to treat it (how do we turn the dial down).
In the meantime watch this helpful video to understand more about the complexity of the pain experience from a world renowned pain neuroscientist: https://www.youtube.com/watch?v=gwd-wLdIHjs
To be continued….
Part 2: Acute vs Chronic pain- Pain as an Alarm!
Part 3: Treatment options for Chronic Pain
References:
Adams, L. M., & Turk, D. C. (2018). Central sensitization and the biopsychosocial approach to understanding pain. Journal of Applied Biobehavioral Research, 23(2), e12125. https://doi.org/10.1111/jabr.12125
Moseley, G. L. (2013). Reconceptualising pain according to modern pain science. Physical Therapy Reviews, 12(3), 169-178. https://doi.org/10.1179/108331907×223010
Moseley, G.L (2003). Unraveling the barriers to reconceptualization of the problem in chronic pain: the actual and perceived ability of patients and health professionals to understand the neurophysiology. https://doi.org/10.1016/S1526-5900(03)00488-7

